Medicines prescribed by a healthcare professional are meant to help you. However, if not consumed or taken care of properly, they may be harmful.
The Know Your Medicine Corner aims to provide you with useful educational information to help you understand the use of medicines better.
We have compiled here common topics on medicine use that are relevant to patients and consumers, helping you to use medicines safely and optimally.
General Medicine Use & Storage

If you are travelling by plane, keep your medicines in your hand-carry luggage.
To help with security at the airport:
- Keep medicines in the original bottles
- Ask your doctor for a copy of all your prescriptions. You may need this in case you misplace, run out, or damage your medicines
- If you have diabetes, ask your doctor for a letter explaining your medical condition with a list of your medications. You are allowed to carry your medicines, blood glucose meter, and lancet device on a plane
- Carry your refrigerated medicines with you on the plane in a cooler bag that is sufficient to keep the medication cold for a few hours. Inform a flight attendant about your medication as soon as you board the long haul flight
- The flight attendant will be able to put the medication in the airplane’s refrigerator. Make sure your container is labeled with your name and contact information
References:
Centers for Disease Control and Prevention. Put Your Medicines Up and Away and Out of Sight. December 12, 2011. www.cdc.gov/Features/MedicationStorage. Accessed on 10 August, 2016.
The Center for Improving Medication Management and the National Council on Patient Information and Education. The quick scoop: medicines and your family: safely storing and disposing of medicines. Updated 2016. www.learnaboutrxsafety.org/quick-scoop.aspx#safely. Accessed 10 August, 2016.
Types of tablet or capsule that you should NOT crush or open:
- Delayed-release or long-acting formulation
Crushing this type of tablet may release the drug all at once. This increases the chance of side effects, the risk of overdosing with the medicines, and potentially a period of time where the drug is not present in your body to exert an effect. - Tablets with a gastro-resistant coating
These tablets contain gastro-resistant granules that are designed to protect the active ingredient from our stomach acid, and are only released when it reaches the intestines.When this gastro-resistant layer is destroyed by crushing, you may increase your chance of a stomach ulcer, have lesser amount of the drug to exert an effect, or stopping the drug from getting to where it needs to work. - Sensitive to light or moisture
Some active ingredients are sensitive to light or moisture (e.g. frusemide is light sensitive). Crushing a tablet or opening a capsule that contains a light- or moisture sensitive active ingredient exposes it to degradation. - Cytotoxic
This group of medicines is toxic to cells as they stop or prevent cells from replicating. They are used to treat cancers and other conditions such as rheumatoid arthritis and multiple sclerosis.It is important that personnel involved in drug preparation or administration are aware of the nature of the drug so that they can avoid unnecessary handling of the drug or take precautionary steps by wearing gloves to prevent skin contact or face mask for inhalation.

Eczema is a skin condition caused by inflammation of the skin. Eczema causes skin to become itchy, red, dry; and sometimes even cracked and leathery.

Moisturizers
- Helps prevent further water loss
- Main role is to prevent eczema from flaring up
- The difference between lotions, creams and ointments is the proportion of oil (lipid) to water
- The higher the lipid content, the thicker the emollient. Hence, the better and longer it works
- The type to use depends on the dryness of your skin, the area of skin involved and your preference:
- Mild skin dryness – Lotion or Cream
- Moderate skin dryness – Cream or Ointment
- Areas of hairy skin – Lotion
Topical Steroids
Topical steroids work by reducing inflammation of the skin and clearing flare-ups.
How to apply moisturizers?
- Use moisturizers at least twice a day, after a shower and before bedtime. They are best applied within 3 minutes after a shower or bath to maximise their moisture-retaining effect
- Apply moisturizers generously to entire body. This prevents the eczema from developing elsewhere
How to apply steroid creams?
- Gently rub the cream or ointment into the skin until it disappears. Then wash your hands (unless your hands are the treated area)
- Overuse of steroids can lead to thinning and discolouration of skin
References
Eczema: How to use Mositurisers and Topical Steroids
Certain medicines are not recommended to be removed from its original packaging and stored in a compliance aid. These include:
- Effervescent tablets
- Dispersible tablets
- Buccal tablets
- Sublingual tablets
- Cytotoxic preparations
Store your medicines in their original containers to preserve their effects as far as possible
If you are required to take half a tablet of your medicine, avoid cutting your pills in advance and storing them in a medication container for later use. This may affect the quality and efficacy of the medication.

Reference
Church, C.; Smith, J. 2006, The Pharmaceutical Journal: “How stable are medicines moved from original packs into compliance aids?”
Sharing of medications is NOT caring
Any medicines will have side effects, but these are known risks and are managed by a health care professional. Thus, the benefits outweigh the risks when the medicine is taken as directed.
It is also important to always seek the advice of a paediatrician before giving medicines to a child. Doses prescribed for adults are not the same for children. Furthermore, certain medications should NOT be given to children because they may harm the child’s development.
Remember that medicines prescribed by your doctor are a choice tailor made for you and your needs. Keep yourself and your family safe by not sharing your medicines.

Reference
Sharing prescription medicines can be bad for health. By Christopher Campbell,Pharm.D, PGY1 Resident, George Regents Medical Center, Augusta; and Christina E. DeRemer Pharm.D., BCPS, Primary Care Clinical Pharmacist & Medicine Team Supervisor, Georgia Regents Health System.

- Proper storage of medicines is crucial to ensure their effectiveness and potency
- Avoid keeping your medicines in your car
- Proper storage areas for example, include your bedroom inside a dresser drawer or in a kitchen cabinet (but keep out of reach of children)
- Make sure the cabinet in the kitchen is not above a stove or a sink, where heat and steam could create moisture problems that will damage the medicines
References
TIPS FOR PROPER STORAGE OF MEDICATIONS Ontario Pharmacists Association
Mistakes in Storage May Alter Medication, By WALECIA KONRADAUG. 15, 2011, http://www.nytimes.com/2011/08/16/health/16consumer.html?_r=0
Not all medicines need to be kept in a refrigerator as they may be adversely affected by the fluctuating temperatures of a domestic refrigerator. Check with your pharmacist for the precise temperature range for your medicines. Only medicines that carry the instruction “REFRIGERATE” should be stored in the refrigerator, preferably in the centre compartment, and to avoid the door or the cooling vent at the back of the refrigerator.
References
TIPS FOR PROPER STORAGE OF MEDICATIONS Ontario Pharmacists Association
Mistakes in Storage May Alter Medication, By WALECIA KONRADAUG. 15, 2011, http://www.nytimes.com/2011/08/16/health/16consumer.html?_r=0

- Types of rectal medications

Rectal Suppositories
Solid, torpedo-shaped pellets that melt at body temperature when inserted into the rectum.

Enemas
Substances in liquid form designed for rectal administration.

Pessaries
Solid, mainly ovoid-shaped preparation for insertion into the vagina (may come with an applicator).
- Method of administration of rectal medications
- Lying position for insertion of rectal suppository or enema.

Adult's position: Lie on the side with the lower leg straightened out and the upper leg bent towards the stomach.
Child's position: Knee to chest, in a crawling position.
Lying position for pessary insertion: Lie on the back, with knees bent, and slightly apart.
- Prior to insertion
- Wash hands and the area of administration with a gentle cleanser/soap and water. Dry it thoroughly.
- Proper technique of insertion
- Insertion of rectal suppository:

- Insertion of pessary:

- Insertion of enema:

- Insertion of rectal suppository:
- Lying position for insertion of rectal suppository or enema.
WHAT IS INSULIN?
Insulin is a hormone made by the pancreas that allows your body to use sugar (glucose) from carbohydrates in the food that you eat for energy or to store glucose for future use. Insulin helps keeps your blood sugar level from getting too high (hyperglycemia) or too low (hypoglycemia).
ARE YOU USING YOUR INSULIN PEN THE CORRECT WAY?
- Get ready: Remove the pen cap from your insulin pen with clean hands.

- Attach the needle: Remove the protective seal and screw the needle on.

- Prime before use: Dial the knob to "2" units and gently tap pen to remove air bubbles.

While holding pen with needle upwards, push the knob until it reaches "0" unit. You should be able to see insulin at the tip of the needle.

- Select the dose: Dial the knob to the required units prescribed.

- Inject your dose: Clean site with alcohol swab, insert needle into skin and press down dial slowly.

Count to 10 before removing.

- Remove the needle: Put outer needle cap back, unscrew and discard used needle.

- Recap insulin pen and store in a safe place at room temperature.

Insulation Injection Sites

SIGNS AND SYMPTOMS OF HYPOGLYCEMIA (LOW BLOOD SUGAR):

Dizziness/Headache

Sweating/Clammy

Blurred Vision

Fast Heartbeat

Hunger
What should you do?
- Check your blood sugar level
- Consume sugar containing beverages e.g. half a glass of fruit juice or 3 teaspoons of white sugar
How to use your metered dose inhaler (MDI)?
- Shake the device by holding it upright with your thumb on the base below the mouthpiece.

- Remove the mouth piece cover.

- If you are using steroid-containing inhalers, remember to gargle your mouth after using the inhaler. Do not swallow the water.
- Breathe out as much as you can, away from the device.

- Repeat the steps after 30 seconds to 1 minute if second dose is required.
- Close your mouth around the mouthpiece to form a tight seal. Do not bite the mouthpiece.

- Breathe in slowly through your mouth. As you do this, press down the top of the canister to release a puff while still breathing in steadily and deeply.

- Hold your breath for at least 10 seconds. While doing so, you can remove the device from your mouth.

Using your MDI with a spacer device
- Remove the cap. Check for any foreign object.

- Insert MDI mouthpiece into the back of the chamber.

- Place the mask onto the mouthpiece end of the spacer.

- Shake the chamber and inhaler 4 to 5 times.

- Press and hold the mask over the mouth and nose. Spray one puff of medicine into the spacer. Breathe in and out for 6 breaths. Repeat this step if a second dose is required.

Mum & Children
Pregnancy is a special physiological condition where the use of medication presents a special concern as the medication may reach the foetus and cause harm. However, total avoidance of medication in pregnancy may not be possible and could be dangerous. Any medicine taken during pregnancy should be used at the lowest effective dose for the shortest possible time.
Tips for medication use during pregnancy
- Never start or stop taking medication before consulting your doctor
- Keep a record of the medication taken during pregnancy or when you are expecting
- Never share your medications
- Do not skip your medication as it may be more harmful to the mother and the foetus
- When in doubt, consult your doctor or pharmacist about the benefits and risks of the medication

References:
Medication and pregnancy. http://americanpregnancy.org/medication/medication-and-pregnancy/
Concerns on Breastfeeding and Maternal Medication Use
Some medication can pass into the breast milk. The amount transferred into the breast milk depends on many factors, including the chemical properties of the medication.
In general, there are very few medications that are absolutely contraindicated during breastfeeding. These medications that present in breast milk may pose risks to the baby while some can affect the supply and composition of the breast milk.
What is “Pump and Dump”?
The “pump and dump” method involves expressing and disposing of the breast milk. It is recommended that this technique be used until at least 3 hours after the last intake of the medicine that is not suitable for use when breastfeeding.
Benefits of this method:-
- Relieves breast fullness or engorgement
- Ensuring breast milk supply
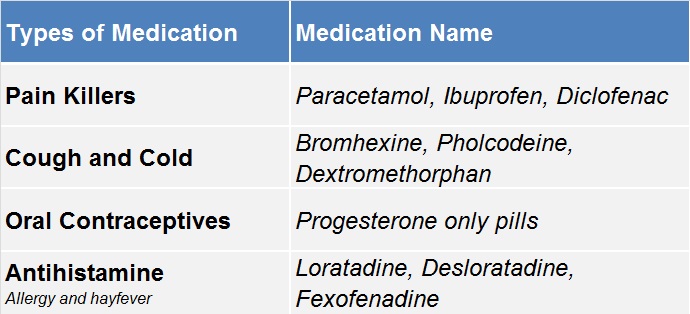
Common Medications Safe for Use during Breastfeeding
How Can Your Pharmacist Help?
Your pharmacist will be able to provide advice on the suitability of your medication and timing to take the medication while breastfeeding, if your medication is safe for your baby or if it may affect your milk supply.
Possible medication timing for consideration
- Immediately after feeding the baby
- Before the baby’s longest sleep period
- After baby’s last feed for the day
References
- BabyCenter. (2017). Drug safety while breastfeeding | BabyCenter. [online] Available at: https://www.babycenter.com/0_drug-safety-while-breastfeeding_8790.bc#articlesection1 [Accessed 3 Sep. 2017].
- Helms, S. and Darbishire, P. (2009). Understanding Breastfeeding: Beyond Medication. US Pharm, 34(9), pp.25-33.
- Verywell. (2017). When to Use the Pump and Dump Method for Lactation. [online] Available at: https://www.verywell.com/pump-and-dump-22415 [Accessed 3 Sep. 2017].
| Definition of Probiotics? |
|
| How Do They Work? |
|
| Probiotics in Food & Supplements |
|
| Prevention & Treatment in Diseases |
|
REFERENCES
- WORLD GASTROENTEROLOGY ORGANISATION GLOBAL GUIDELINE – PROBIOTICS AND PREBIOTICS 2017.
- LIPPINCOTT WILLIAMS & WILKINS. CLINICAL EFFICACY OF PROBIOTICS: REVIEW OF THE EVIDENCE WITH FOCUS ON CHILDREN. JOURNAL OF PEDIATRIC GASTROENTEROLOGY AND NUTRITION.43:550-557. OCTOBER 2006.
- DAN W.THOMAS ET AL. AMERICAN ACADEMY OF PAEDIATRICS.CLINCAL REPORT- PROBIOTICS AND PREBIOTICS IN PEDIATRICS. VOLUME 126,NUMBER 6. DECEMBER 2010.
FAQ on Probiotics
What does CFU mean?
CFU stands for “colony forming units” and is used to quantify how many bacteria in probiotics are capable of dividing and forming colonies.
Does more CFU mean better?
The dose needed for probiotics varies greatly depending on the strain and product although many are in the range of 1–10 billion CFU per dose.
Do probiotics have side effects?
Side effects are typically mild, temporary and often a sign that the probiotics are working and are often part of the natural cleansing process, for example, minor constipation, mild diarrhoea, mild rash, cramps, and gas.
How long do I need to take probiotics?
It is recommended to take probiotics daily between 2 weeks to 2 months to fully re-colonize the bowel’s healthy bacteria.
Are probiotic supplements safe for pregnant or nursing mothers?
Probiotic supplementation during pregnancy improves newborn’s immunity and decreases allergies. For nursing infants, immunity and allergy improvements have also been observed. Always check with your doctor or pharmacist to confirm that any supplement, including probiotics, are safe for use during pregnancy and breastfeeding.
REFERENCES
World Gastroenterology Organisation Global Guideline – Probiotics and Prebiotics 2017
Patient handout. University of Wisconsin Integrative Medicine

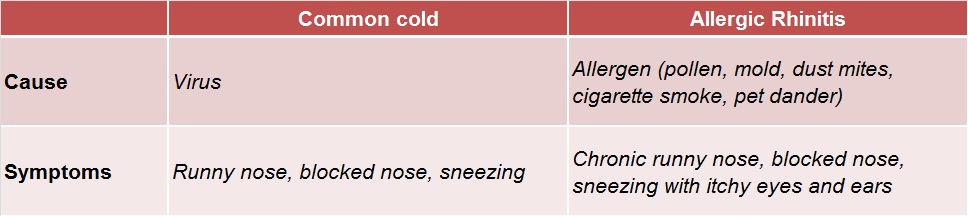
Allergic rhinitis can affect school work and sports performance
- The nasal congestion caused by allergic rhinitis may affect the child’s quality of sleep. This would affect their concentration the following day
- As the child’s breathing quality is affected, their ability to exercise and play sports is also compromised
What are the management strategies for allergic rhinitis?
Besides seeking medical attention, the first approach is to identify the triggers and minimize exposure.
Outdoor exposure
- Wear mask and glasses
- Avoid hanging clothes outside
Indoor exposure
- Mites – use “mite-proof” covers, wash linens and curtains with hot water
- Mould – use dehumidifier
Pet dander exposure
- Wash hands after petting animals
- Keep pets outside

Nasal irrigation is used to rinse off the allergens and is effective in approximately 50% of patients with allergic rhinitis.
Reference
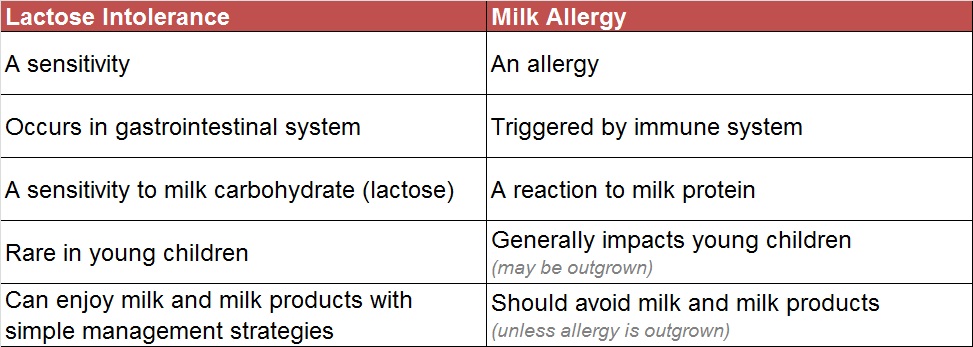
What is Lactose Intolerance?
Lactose intolerance is when the body cannot digest lactose which results in gastrointestinal symptoms.
What causes lactose intolerance?
- It occurs when the small intestines do not produce enough lactase (enzyme) to digest lactose (milk sugar). Lactose is then fermented by bacteria and produces unpleasant symptoms
- Lactose intolerance in children is often caused by an infection in the digestive system, and will only last a few weeks

What are the symptoms of lactose intolerance?
Symptoms of lactose intolerance usually occur within 30 minutes to 2 hours after lactose consumption and includes:

What types of food contain lactose?
- Lactose is the natural sugar found in the milk of mammals such as cows, goats and sheep
- Dairy products such as cheese, ice cream, butter and yoghurt may contain lactose
How is lactose intolerance managed?
- There is no cure for lactose intolerance. However, symptoms can be reduced by making changes to diet
- Serve small servings of milk and dairy products in regular meals
- For babies with lactose intolerance, lactose-free formula milk is available in pharmacies and supermarkets
- Probiotics may help in the management of lactose intolerance
Is lactose intolerance the same as milk allergy?
No. They may share similar symptoms but are entirely different conditions
References
- http://www.mayoclinic.org/diseases-conditions/lactose-intolerance/basics/definition/con-20027906
- https://www.niddk.nih.gov/health-information/digestive-diseases/lactose-intolerance
- https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Lactose-Intolerance-in-Children.aspx
- http://www.nhs.uk/Conditions/lactose-intolerance/Pages/Introduction.aspx
Safe Use of Antibiotics
Most cough and cold illnesses are caused by viruses. Antibiotics can only treat bacterial illnesses–not viral illnesses.
Common illnesses where antibiotics are NOT REQUIRED include:
- Colds
- Influenza (the flu)
- Runny noses
- Most coughs
- Most sore throats
- Most sinus infections
- Some ear infections
How long will the symptoms last?
 |
Sore throat / tonsillitis: 1 week |
 |
Cold / flu: 10 days – 2 weeks |
 |
Runny / blocked nose: 1 – 3 weeks |
 |
Sinusitis: 2 – 3 weeks |
 |
Dry / tickly cough: 3 weeks |
If symptoms last longer than normal, do not improve, get worse or if new symptoms develop, seek medical advice.
How do I know if I have a viral or bacterial infection? Consult healthcare provider and follow his or her advice on what to do about the illness. Remember, common colds are caused by viruses and do not require antibiotics.
Does this mean I should never take antibiotics? Your healthcare provider will prescribe antibiotics if you have a bacterial infection.
If mucus from nose changes from clear to yellow or green – does this mean that I need antibiotics? No. It is normal for mucus to get thick and change colour during a viral cold.
What can I do to help myself feel better? Pain relievers, fever reducers, saline nasal spray or drop, warm compress, liquids and rest may be the best things to help you feel better.

References:
- Snort. Sniffle. Sneeze. No Antibiotics Please. Centres for Disease Control and Prevention (CDC).
- Get to the source of Cold & Flu symptoms. Global Respiratory Infection Partnership (GRIP).
- Upper Respiratory Tract Infections Getting the right relief. Global Respiratory Infection Partnership (GRIP).
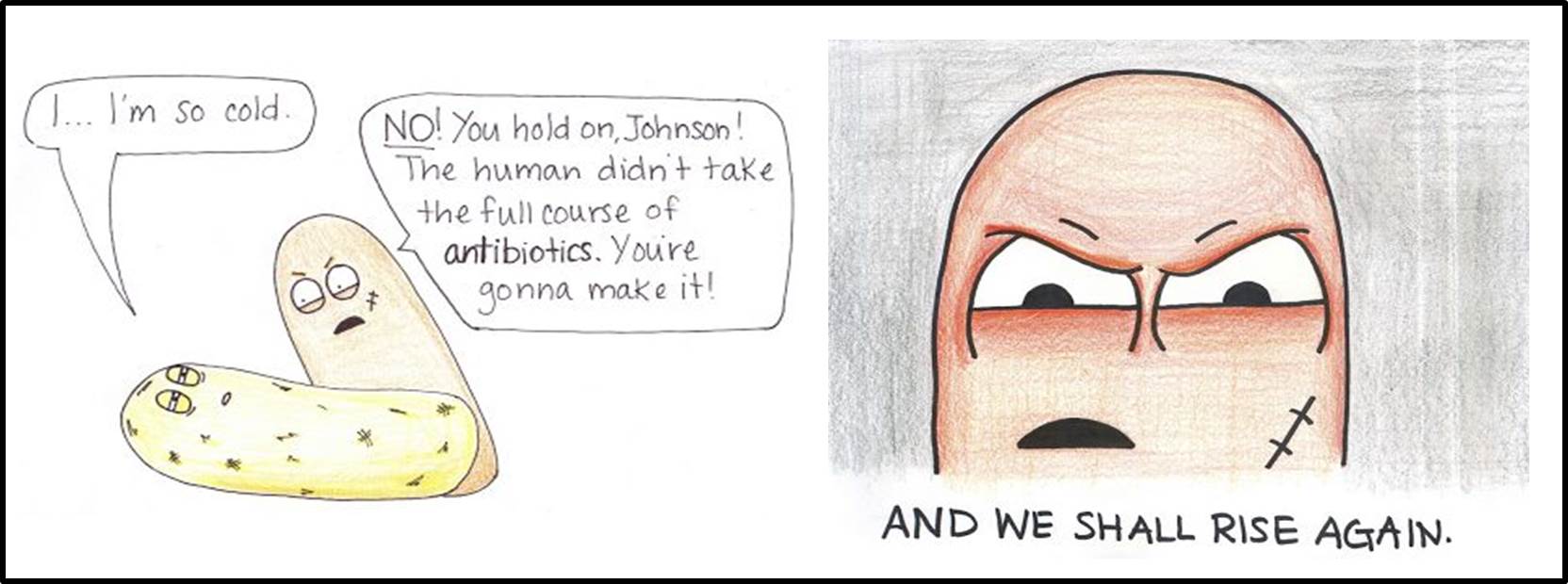
Why should I finish my antibiotic?
Not finishing a course of antibiotics as directed can lead to *antibiotic resistance.
*Antibiotic resistance is resistance of the bacteria to the antibiotic that was originally effective for treatment of infections caused by it. Illnesses that were once easily treatable with antibiotics become dangerous infections, prolonging suffering and may even be fatal.
YOU can help tackle resistance by:
- Hand washing and avoiding close contact with sick people to prevent transmission of bacterial infections;
- Use antibiotics only when they are prescribed by a certified healthcare professional;
- Completing the full treatment course, even if you feel better;
- Never share antibiotics with others or use leftover prescriptions

I developed diarrhoea after taking antibiotics. Should I stop it?
In some patients, antibiotics may cause mild diarrhoea, which is a well known effect. You do not need to discontinue your antibiotic but well hydrate yourself to replace the lost fluids and avoid milk containing products.
Probiotics are recommended to help with diarrhoea. However if you develop severe abdominal pain, cramps or fever with high volume diarrhoea after taking antibiotics, you should seek your doctor’s attention immediately.
I developed an allergy reaction towards penicillin. Is it safe for me to take other antibiotics?
If you developed itchiness, difficulty breathing and/or wheezing after taking penicillin, then you are allergic to it and you should not take any product containing penicillin or an antibiotic of a similar class.
It is important that you notify any doctor or pharmacist that looks after you on your allergy status. There are other antibiotics available which are safe to use for people with penicillin allergy.
References
Reporting Of Medicine Side Effects by Consumers
What Is A Side Effect/Adverse Drug Reaction?
- An unwanted effect or a harmful reaction experienced following the administration of a drug/medicine or combination of medicines
- The reaction may be a known side effect of the medicine or it may be new and previously unrecognised
- It can also suddenly occur with medicines that you have taken often without side effects previously

Some Examples of Side Effects

Rashes

Nausea, vomiting

Difficulty in breathing

Swelling (lips, eyes & tongue)
Step 1
If you believe you are having a side effect, it is important to speak/see your doctor or pharmacist.
Step 2
- Report to the National Pharmaceutical Regulatory Agency (NPRA)
- Use ConSERF (Consumer Side Effect Reporting Form). Please report any side effect you find troubling, even if you are not certain it is due to the medicine
Please note down the following information:
- Drug Name
- Dosage Taken
- Duration of drug taken until side effect occurred
- Name of other drugs taken at the same time
How To Report?
- Please complete as many sections as possible to ensure your report is useful. You may consult your pharmacist for assistance in filling the form
- Submit online, or post/email directly to NPRA
- Please provide your contact details to allow NPRA to obtain further information about your report if necessary. Your details will remain confidential
Role of NPRA, Ministry of Health Malaysia
The National Pharmaceutical Regulatory Agency (NPRA) monitors the safety of medicines in Malaysia to contribute to a better understanding of their possible side effects. Analysis of side effect reported has contributed to the following steps to improve medication safety:
- Issuing safety alerts & prescribing restriction of at-risk medicine
- Updating the package inserts & consumer medicine information leaflets with the latest safety information
- Removal of certain at-risk medicine from the market
What To Report?
You can report side effects from:
- Medicines or vaccines (prescription medicines from the doctor or over-the-counter medicines)
- Vitamins and health supplements
- Herbal or traditional medicines
Besides oral medicines (tablets, capsules and syrups); other medicines like creams, lotions, suppositories and inhalers can also cause side effects.
Role of NPRA, Ministry of Health Malaysia
Unfortunately it is impossible to know all side effects of a medicine before it is approved for use. When people report about their experiences using a particular medicine it helps us to understand more about the possible side effects of the medicine and identify new problems that we might not have known before.
What Is A Drug Allergy?
- A drug allergy is an undesirable effect occurring as a result of the body’s immune response to a drug
- Allergic reactions due to medications do not happen to everyone
What Are The Symptoms of Drug Allergy?
Symptoms may vary from one patient to another.
Mild allergic reactions:
- Skin rashes or urticaria (hives)
- Repeated-itching
ANAPHYLAXIS – life-threatening and requires urgent medical attention!
- Skin rashes or urticaria (hives)
- Itching
- Itching

Drugs commonly associated with allergic reactions:
- Antibiotics – penicillin (cloxacillin, amoxycillin), trimethoprim/sulphamethoxazole
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) – mefenamic acid, ibuprofen, diclofenac
What should you do if you think you have a drug allergy?
If you know or suspect you are allergic to a drug:
- AVOID / STOP taking that drug
- Seek medical advice from your doctor to confirm the allergy
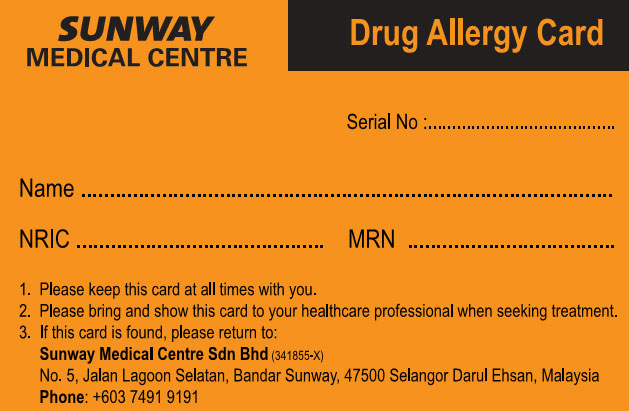
DRUG ALLERGY CARD
- Useful for patients with confirmed drug allergy
- Alerts healthcare professionals about a patient’s drug allergies
- Helps prevent patients from taking drugs that may cause allergic reactions
Tips for allergy card holders:
- Bring along the drug allergy card at all times
- Show the drug allergy card to any healthcare professionals involved in your care
- For severe allergic reactions, consider obtaining a medical alert bracelet
DRUG ALLERGY
A drug allergy is a rare condition in which the body’s immune system responds to a drug and causes adverse effects
SIDE EFFECT
A side effect to a drug is:-
- an unwanted effect from a drug
- different from a drug allergy
- does not involve an immune reaction

*Sometimes a side effect to a drug may disappear as drug therapy continues
Glucose-6-Phosphate Dehydrogenase (G6PD) Deficiency

What is G6PD?
G6PD, also known as glucose-6-phosphate dehydrogenase, is an enzyme which helps the body convert sugar to energy. It is found in all cells of the body, but mainly in red blood cells.
Function of G6PD Enzyme
These enzymes help protect haemoglobin in red blood cells from harmful chemicals, to carry oxygen througout the body.
G6PD Deficiency
Deficiency of G6PD enzymes does not usually cause problems or symptoms.
It may, however, become a problem if the person is exposed to certain chemical compounds, or experience certain infections that can cause cells to be destroyed in a process known as haemolysis.
Consequences of G6PD Carriers
People with G6PD deficiency are at increased risk of haemolysis and severe anaemia, due to the breakdown of haemoglobin upon chemical exposure. This condition is known as haemolytic anaemia.
Symptoms of this condition includes pale skin, yellowing of the skin/eyes, dark-coloured urine, fever, dizziness and confusion. Hence, in some cases, short-term treatment involving fluids or blood transfusions may be required.
Preventive Actions by G6PD Carriers
G6pD deficiency is best managed by preventative measures through avoiding certain medications or food. By doing so, serious symptoms can be prevented.
Medications that are known to 'trigger' haemolysis and should be avoided can be found in Figure 1.


Figure 1